Member plans and coverage
Member plans, or insurance plans, must be reviewed and evaluated to determine a patient's medical coverage for a program. The coverage investigation process, which includes benefits verification, subsequently identifies patients who are eligible to enroll in assistance programs.
Note
"Member plan" and "insurance plan" may be used interchangeably. Patients are plan members of insurance providers.
Relating to care plans
The Member Plan (mvn__PJN_Member_Plan__c) custom object stores information about a patient's insurance plan(s), including details like the name and type of each plan.
Member plans are related to care plans via the PJN_CarePlanLookupMapping Apex class as well as the Care Plan Lookup Mapping (mvn__PJN_Care_Plan_Lookup_Mapping__mdt) custom metadata type. Komodo Care Connect provides three Care Plan Lookup Mapping records in the initial installation script to identify the primary, secondary, and tertiary member plans on a care plan:
Set Primary Member Plan (
PJN_Set_Primary_Member_Plan)Set Secondary Member Plan (
PJN_Set_Secondary_Member_Plan)Set Tertiary Member Plan (
PJN_Set_Tertiary_Member_Plan)
When a member plan is identified as a primary, secondary, or tertiary member plan via the mvn__PJN_Coverage_Order__c field on the Member Plan record, the trigger class and mapping records stamp the member plan onto the appropriate mvn__PJN_Primary_Prescription__c, mvn__PJN_Secondary_Prescription__c, or mvn__PJN_Tertiary_Prescription__c field on the Care Plan (Case) record. The corresponding mvn__PJN_Set_as_Primary__c, mvn__PJN_Set_as_Secondary__c, or mvn__PJN_Set_as_Tertiary__c field as well as the mvn__PJN_Active__c field on the Member Plan record are both subsequently updated as well.
If the coverage order of a member plan changes such that the mvn__PJN_Coverage_Order__c field on the Member Plan record is updated, all respective lookups on the Care Plan record are reset via the PJN_ClearMemberPlanFields Apex class. They are then updated by the PJN_CarePlanLookupMapping Apex class again.
Relating to coverage investigations
Information about the coverage provided and the out-of-pocket costs required by each member plan is stored in the Coverage Benefit (mvn__PJN_Coverage_Benefit__c) custom object. Each Coverage Benefit record looks up to a Member Plan record.
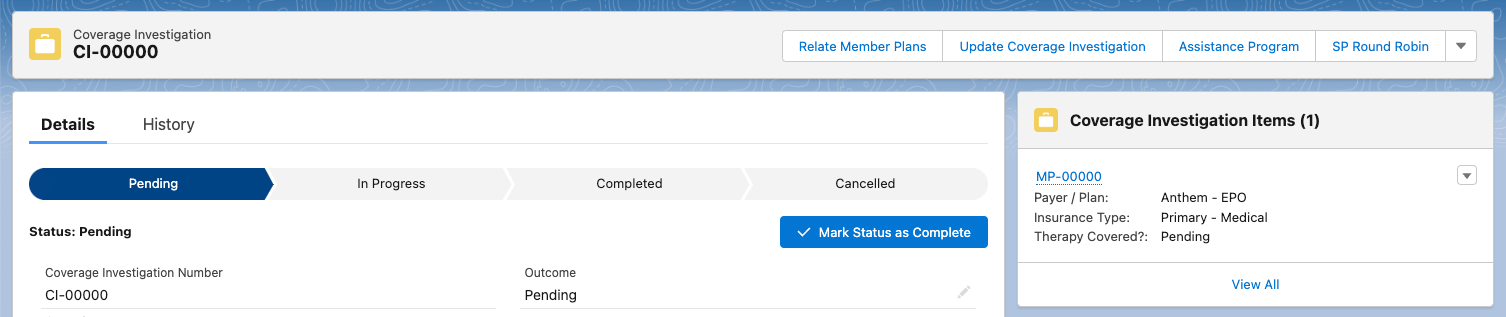
Meanwhile, information about the coverage investigation process and outcome for each member plan is stored in the Coverage Investigation (mvn__PJN_Coverage_Investigation__c) custom object. However, Member Plan records do not relate directly to Coverage Investigation records. Instead, Member Plan records relate to Coverage Investigation records via the Coverage Investigation Item (mvn__PJN_Coverage_Investigation_Item__c) junction object. This allows member plans to be related to multiple coverage investigations.
For users, the relation to and from the Coverage Investigation Item record is automatic when creating and updating a coverage investigation. Once a coverage investigation is created and one or more member plans are selected, the member plans will be related to and appear under the coverage investigation item of the coverage investigation. Coverage investigations can be created before or after member plans are created.
Note
All other items pertaining to a coverage investigation, such as a prior authorization that may need to be completed during the investigation process or an assistance program that eligible patients can enroll into after the investigation process, are managed in other custom objects. These objects, such as Assistance Program (mvn__PJN_Assistance_Program__c) and Prior Authorization (mvn__PJN_Prior_Authorization__c), can relate directly to a Coverage Investigation record.
Out of the box, if you create a Prior Authorization record from a Member Plan record that is related to a Coverage Investigation (mvn__PJN_Coverage_Investigation__c) record and the Coverage Investigation record has a Status (mvn__PJN_Status__c) value of Pending or In Progress, the prior authorization will automatically be related to the coverage investigation. This is managed by the Prior Authorization: KCC Before Insert (mvn__PJN_Prior_Authorization_Before_Insert) flow.
Relate to new coverage investigation
When users create a new coverage investigation on a care plan, they must indicate whether it is an initial investigation or a re-authorization of a previous investigation. If the former, and one or more member plans already exist on the care plan, some member plans may be automatically selected to be included in the coverage investigation. Users can deselect these as appropriate.
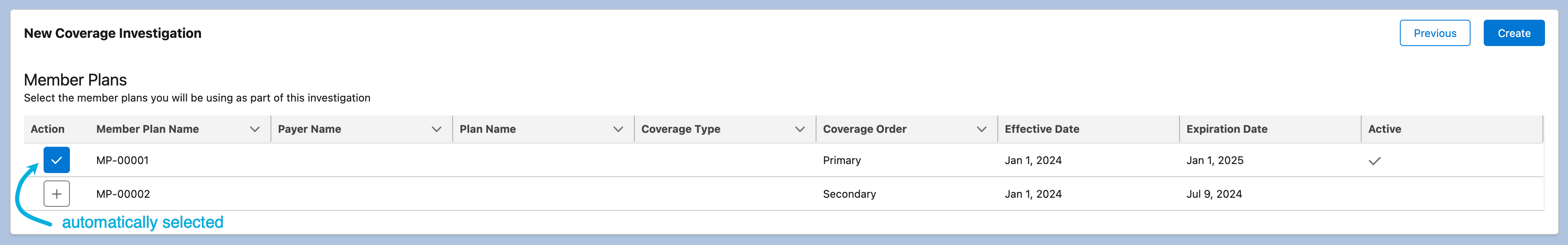
Out of the box, all active member plans, or Member Plan records whose Active (mvn__PJN_Active__c) field equals true, are automatically selected for initial investigations via the Active Indicator Fields (mvn__PJN_Active_Indicator_Fields) field set. To modify the criteria that evaluates which Member Plan records are automatically selected for an initial coverage investigation, add or remove fields from this field set. If any of the fields in the field set equals true on the Member Plan record, then the member plan will be automatically selected. For example, if you have a custom Active field in addition to the standard Active field on the Member Plan object to identify active member plans for a patient and you add both fields to the Active Indicator Fields field set, if either the custom Active field or the standard Active field equals true for the Member Plan record, then the member plan will be automatically selected for the initial coverage investigation.
Relate to existing coverage investigation
If a member plan is created after a coverage investigation is created or if a member plan is missing from an existing coverage investigation, users can still add the member plan to the coverage investigation. Out of the box, users can click Relate Member Plans (PJN_Relate), which is managed by the PJNCoverageInvestigationQuickAction Lightning Component, in the highlights panel of the PJN Coverage Investigation page layout and then select the member plan as appropriate.
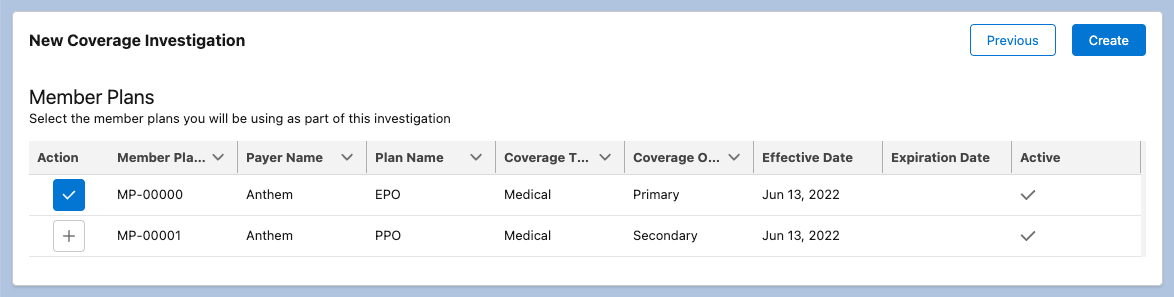
Configuration
The columns that appear in the New Coverage Investigation screen as well as the Update Coverage Investigation screen via the PJNCoverageInvestigationQuickAction Lightning Component are managed by the Coverage Investigation Add Screen (mvn__PJN_Coverage_Investigation_Add_Screen) field set in the Member Plan (mvn__PJN_Member_Plan__c) object.
Updating coverage investigations
Out of the box, users can modify coverage investigations in two ways, both of which are available in the highlights panel of the PJN Coverage Investigation page layout:
Via the standard Edit button
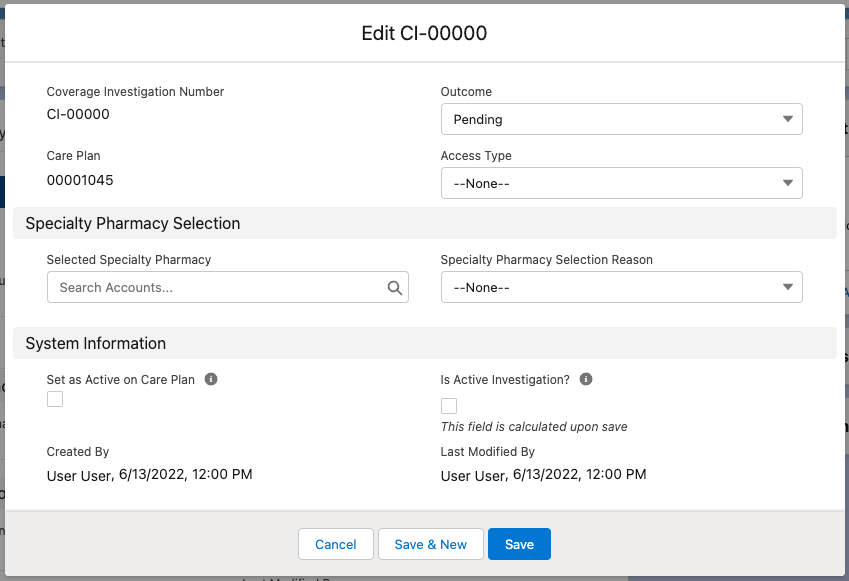
Via the custom Update Coverage Investigation (
PJN_Update_Coverage_Investigation) button, which is managed by thePJNCoverageInvestigationUpdateQuickActionLightning Component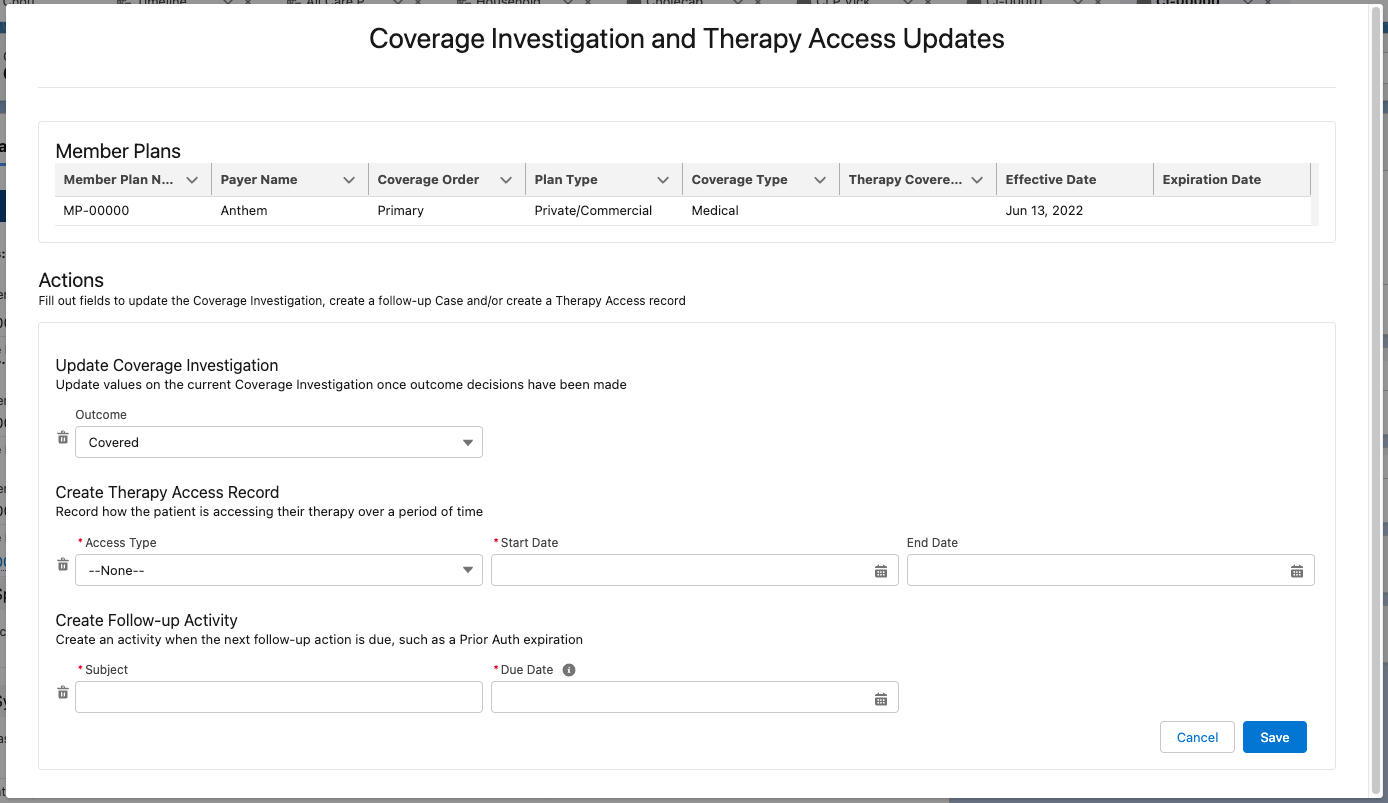
While both options enable users to update the outcome and access type of a coverage investigation, the latter offers an extensive view of all the coverage investigation items included in the coverage investigation. It also allows users to record the effective period of and add follow-up activities for a therapy access. The component and modal can be further configured using the field sets on the following objects:
Section | Object API name | Field set API name |
|---|---|---|
Member Plans | mvn__PJN_Member_Plan__c | mvn__PJN_Coverage_Investigation_Update_Screen |
Prior Authorizations | mvn__PJN_Prior_Authorization__c | mvn__PJN_Coverage_Investigation_Update_Screen |
Assistance Programs | mvn__PJN_Assistance_Program__c | mvn__PJN_Coverage_Investigation_Update_Screen |
Update Coverage Investigation | mvn__PJN_Coverage_Investigation__c | mvn__PJN_Coverage_Investigation_Update_Screen |
Create Therapy Access Record | mvn__PJN_Event__c | mvn__PJN_Coverage_Investigation_Update_Screen |
Create Follow-up Activity | Case | mvn__PJN_Coverage_Investigation_Update_Screen |